Compassionate, Culturally Attuned Care for Depression, Anxiety, and Beyond
Across Southern Arizona, many families seek reliable, evidence-based help for depression, Anxiety, and related challenges that can disrupt school, work, and relationships. From Green Valley to Tucson Oro Valley, and from Sahuarita to the border communities of Nogales and Rio Rico, access to comprehensive mental health care transforms lives when it blends science, compassion, and community awareness. People deserve care that meets them where they are—and that spans prevention, therapeutic intervention, and sustained recovery.
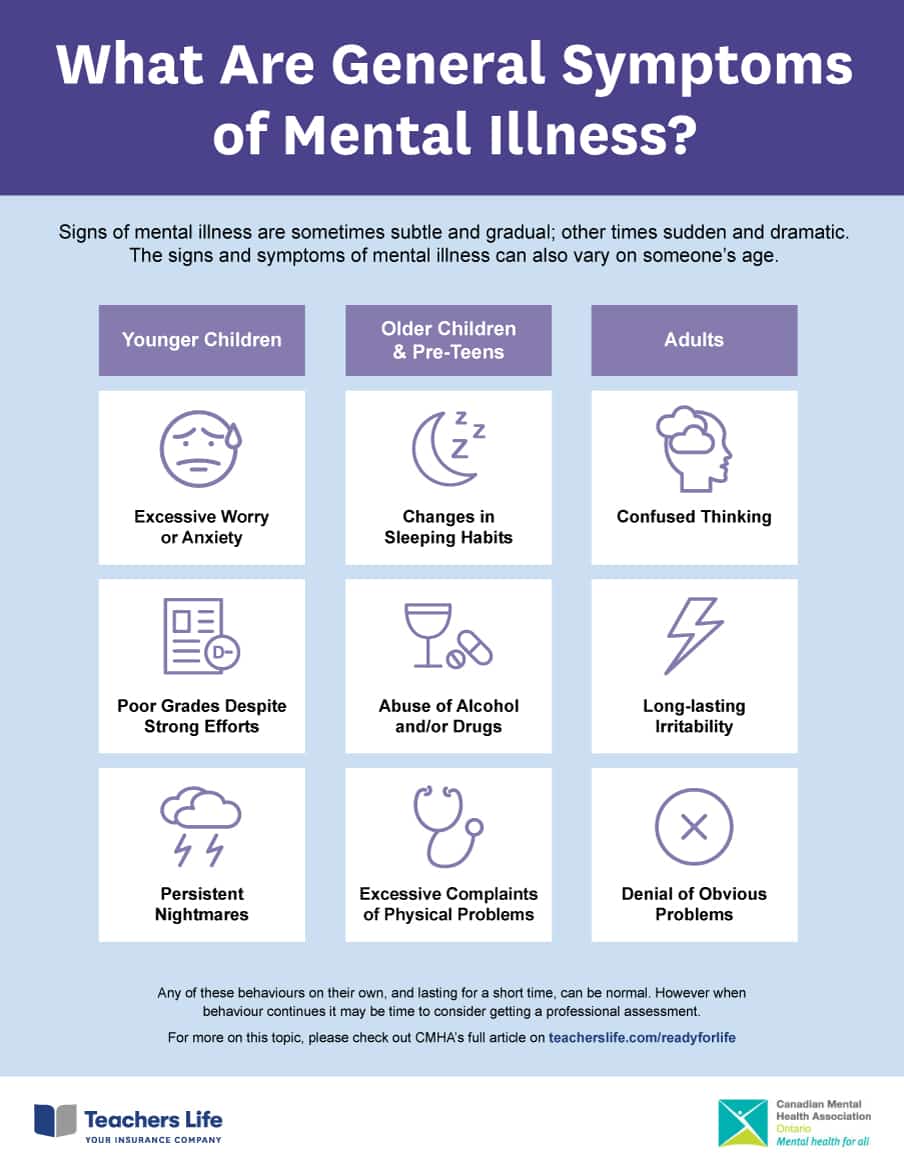
For adults and children, high-quality therapy weaves together approaches matched to the person’s goals and symptoms. Skilled therapists may use CBT to address thought patterns fueling sadness, anger, or worry; EMDR to process trauma memories that keep the body on high alert; and mindfulness-based strategies to calm the nervous system during panic attacks. When symptoms are more complex—such as co-occurring mood disorders and eating disorders, or persistent insomnia—plans expand to include sleep hygiene, nutritional support, and skills training for distress tolerance and interpersonal effectiveness.
Integrated med management helps stabilize mood and reduce intrusive symptoms while therapy builds resilience. Thoughtful prescribing accounts for medical history, family genetics, and personal preference. Patients and families are engaged in clear conversations about benefits and side effects, and treatment is carefully adjusted over time. This collaborative model is especially important for conditions like OCD, PTSD, and Schizophrenia, where a synchronized team approach improves adherence, safety, and quality of life.
Care also needs to be accessible. Spanish Speaking services ensure bilingual families can share their stories fully and understand treatment options without the barrier of translation. Therapists and medical prescribers familiar with regional realities—cross-border stressors, seasonal work, extended family dynamics—create plans that are realistic and respectful. Whether meeting a teen from Tucson Oro Valley navigating social anxiety, a parent in Sahuarita managing work stress and grief, or an elder in Green Valley living with isolation, a connected, culturally sensitive approach opens the door to sustained healing.
Deep TMS, BrainsWay, and Evidence-Based Psychotherapies Working Together
When traditional treatments do not sufficiently ease symptoms, modern neuromodulation offers powerful options. Deep TMS uses magnetic fields to gently stimulate neural networks implicated in depression, AnxietyBrainsWay deliver targeted stimulation through coils designed to reach deeper brain regions than standard TMS, potentially benefiting people who have tried multiple antidepressants without relief. Sessions are noninvasive, require no anesthesia, and have minimal side effects—typically a tapping sensation or mild scalp discomfort that fades quickly.
What makes this especially effective is integration. Neuromodulation is not a standalone fix; it is most potent when paired with active psychotherapy and lifestyle strategies. During a course of Deep TMS, therapists often coordinate CBT to reinforce new thinking patterns and behaviors as mood improves. For trauma-related symptoms, EMDR can be scheduled to process distressing memories once hyperarousal decreases. As attention, energy, and sleep stabilize, patients can commit more consistently to therapeutic goals, strengthening gains.
Thoughtful med management continues alongside TMS, with careful adjustments to avoid overmedication and to maximize synergy. For instance, a patient with treatment-resistant depression who experiences partial response to BrainsWay Deep TMS may taper off an ineffective agent while introducing a more targeted option. In conditions like OCD, exposure and response prevention can be paired with neuromodulation to improve tolerance for uncertainty and reduce compulsive rituals. For psychosis-spectrum symptoms or Schizophrenia, the focus shifts to stabilization, insight building, and community supports, while exploring whether neuromodulation is appropriate on a case-by-case basis.
Families often ask how long results last. Sustained outcomes depend on the whole ecosystem of care—follow-up boosters when indicated, consistent therapy, sleep and nutrition, movement, and connection. Many people in Nogales and Rio Rico report renewed motivation and the ability to resume work or school after a structured course. For teens and children, family sessions help communicate needs clearly and set boundaries around technology, sleep routines, and social commitments. This integrated model gives people a realistic path toward recovery—structured, individualized, and grounded in science.
Real-World Stories: From Panic to Progress in Green Valley, Sahuarita, Nogales, and Beyond
Consider a college student from Tucson Oro Valley whose escalating panic attacks made classes impossible. Weekly CBT targeted catastrophic thinking and avoidance, while a brief medication trial reduced baseline autonomic arousal. After learning diaphragmatic breathing and graded exposure, the student practiced entering crowded lecture halls with support. Within eight weeks, panic frequency declined by more than half. A subsequent round of EMDR addressed a prior car accident that had been feeding hypervigilance. Grades recovered, and social life stabilized because treatment addressed both the biological and experiential roots of fear.
In Sahuarita, a parent living with chronic depression and insomnia tried multiple medications without lasting relief. A course of Deep TMS using a BrainsWay system was added to the plan, synchronized with CBT for insomnia and gentle activity scheduling. Week by week, energy lifted; the ability to enjoy family time returned. With guidance on med management, unnecessary polypharmacy was reduced, side effects diminished, and the parent regained clarity to engage in values-based goals.
In Nogales and Rio Rico, culturally attuned, Spanish Speaking counseling supports families facing intergenerational stress, PTSD, and migration-related loss. One family sought help for a teen with binge-restrict cycles and body dissatisfaction. A combination of family-based therapy for eating disorders, nutritional counseling, and medical monitoring safeguarded health while addressing perfectionism and identity. The bilingual team normalized conversations about food, culture, and belonging—core elements that a purely symptom-focused model can miss.
Leadership and community engagement matter. Clinicians like Marisol Ramirez foster trust through outreach, education, and care that respects each person’s story. Community programs such as Lucid Awakening connect people to resources spanning therapy, peer support, and advanced interventions. For individuals with mood disorders, OCD, or complex trauma, these networks reduce isolation and strengthen continuity. In Green Valley, elders often benefit from grief counseling and social activation; in Tucson Oro Valley, teens find safe spaces to learn coping skills; in Sahuarita, parents receive coaching for stress regulation and communication. By aligning science-backed interventions with local strengths—family, culture, resilience—healing becomes more than symptom reduction; it becomes a practice of living well in community.
These stories illustrate a shared path. Whether confronting Schizophrenia with structured supports, rebuilding after PTSD with phased trauma care, or resolving OCD rituals through exposure work supplemented by neuromodulation, progress accelerates when treatments converge. With accessible care in Green Valley, Tucson Oro Valley, Sahuarita, Nogales, and Rio Rico, and with options ranging from psychotherapy and med management to Deep TMS and EMDR, people reclaim momentum and meaning—one grounded step at a time.